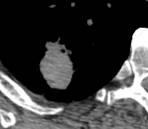
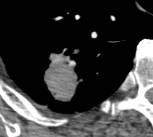
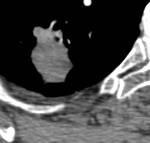
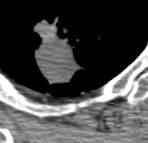
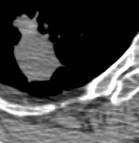
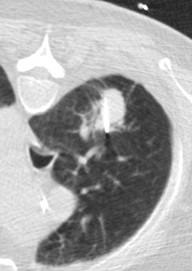
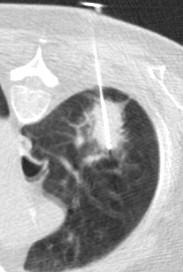
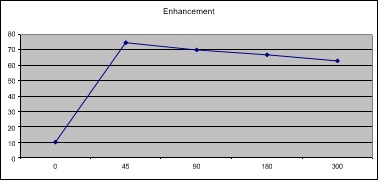
Recurrence after RFA Brown university ExperienceTo review the recurrence patterns in patients with primary non-small cell lung cancer (NSCLC) treated with percutaneous image-guided radiofrequency (RF) ablation. 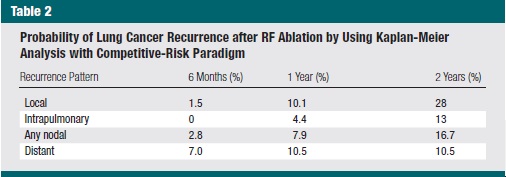 The most common pattern of recurrence was local, which suggests that more aggressive initial RF ablation and adjuvant radiation may offer improvement in outcomes. Continued follow-up imaging is needed because new recurrences were seen throughout the 2 years following treatment. 在所有复发类型中,局部复发占比28%,是通过加强首次射频消融或配合辅助放疗,加强CT随访,因为新复发通常贯穿2年时间 Michael D Beland Primary Non-Small Cell Lung Cancer: Review of Frequency, Location, and Time of Recurrence After Radiofrequency Ablation Radiology 254 (1), 301-7 2010(free) Possible recurrence:射频消融术后第3个月增强CT随访
Repeat RFA “Touch-up” for Residual NSCLC
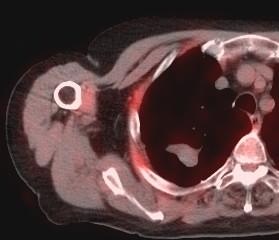
Follow-up CT and PET/CT
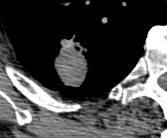
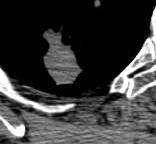
Repeat radiofrequency ablation for local progression of lung tumors: does it have a role in local tumor control?
To retrospectively evaluate the role of repeat radiofrequency (RF) ablation for local progression of lung tumors in local tumor control.
- 797 tumors treated- 66 NSCLC
- 50 repeat RFA in 56 tumors- 9 NSCLC
- Secondary effectiveness rate (SER) for uncomplicated cases was 94% at 1yr, 68% at 2yrs, and 55% at 3yrs
- SER for complicated tumors 60% at 1yr and 40% at 2yrs
- (P<.00001) compared with PER(primary effectiveness rate?)
Conclusions
Repeat RF ablation improved the overall local control outcomes. In particular, it offered an opportunity to salvage tumors【1】 that had no risk factors but nevertheless progressed locally after the first RF ablation. Conversely, tumors with risk factors were not controlled sufficiently even after repeating the procedure.
【1】The term “salvage (or ‘rescue’) surgery” has been used to refer to surgical treatment after failure of initial treatment in various scenarios including treatment of delayed neck metastasis, recurrent primary tumors, or even lung metastasis. The first reference to “salvage surgery” for oncologic treatments found on PubMed was to surgical treatment for lack of response after adequate management of primary tumor with radiotherapy, published in 1965 [1]. In the treatment of head and neck cancer, the first reports from the 1970s refer to “salvage” in the form of a laryngectomy or pharyngolaryngectomy following radiotherapy [2, 3]. This concept was defined from trials which offered exclusive radiotherapy or radiochemotherapy [4, 5] for patients with advanced head and neck tumors. Such patients will have two different outcomes: many will achieve a complete response after the non-surgical therapy and will not need further treatment, while some of them will have a partial response which will need a complement of the original treatment, to “rescue” them from the failure of the first treatment. However, with the introduction of newer treatment protocols, such as organ preservation schemes, and with knowledge of the outcomes of most tumors initially submitted to non-surgical therapies, the indications for “salvage surgery” have increased, but without a concomitant evolution of the term. Since the first description of salvage surgery after radio(chemo)therapy protocols, the number of publications related to the subject have increased dramatically. Salvage surgery is no longer limited to patients who failed radiotherapy or radiochemotherapy, but also includes patients who previously underwent surgical treatment for tumors located from the base of the skull to the lower neck areas (including thyroid cancer).
Hiraki T, et al Repeat Radiofrequency Ablation for Local Progression of Lung Tumors: Does It Have a Role in Local Tumor Control? J Vasc Interv Radiol. 2008 ;19:706-11
|

|