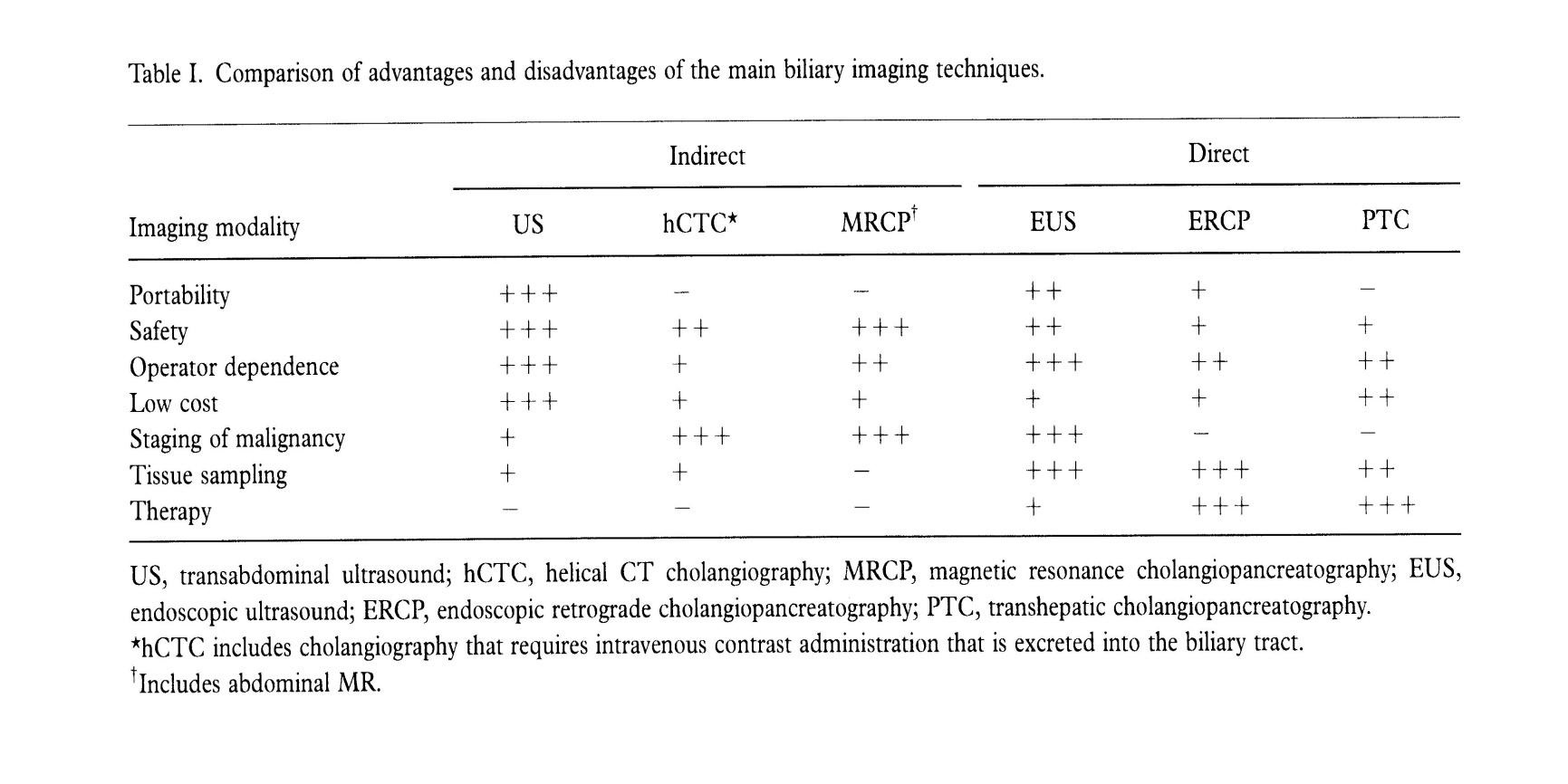
根据 Clinical History; Physical exam 和 Laboratory tests,可以诊断大约90%的梗阻性黄疸。影像学的主要任务是: 1. 确定诊断 2. 决定梗阻的水平 3. 查明病因 4. 制定治疗计划 传统诊断梗阻性黄疸主要依赖PTC,经皮胆道造影;随着影像学的进步,PTC is dead。
The answer is clear in both ways:
Yes, the PTC is dead as a diagnostic method when we suspect a biliary obstruction, because today, except in rare cases , there are more modern non-invasive imaging methods which obtain very good results.
And no, because it s crucial as a first step as a part of a therapeutic method of biliary drainage, percutaneous management of benign and
malignant stenosis, and stone removal.
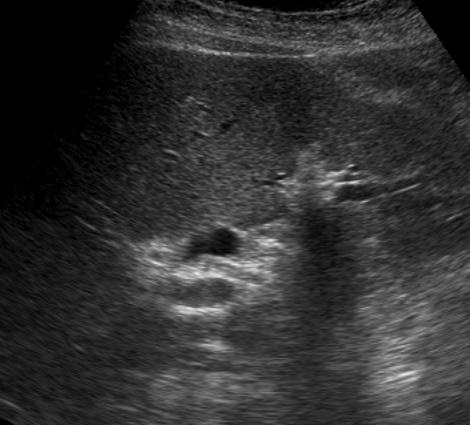
Imaging techniquesNot interventional, or indirect techniquesAbdominal ultrasound (USab)
First choice technique in BO:
- Non-aggressive, inexpensive,and available
BO criteria: BT >8mm
- Absent : does not exclude BO
- Dilated choledoco without BO
Advanced age or following cholecystectomy
Operator dependent
Less precise:
- Level of BO; published data 27- 95%
- Cause of BO published data 23 - 88%
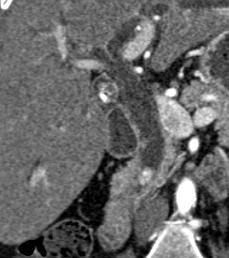
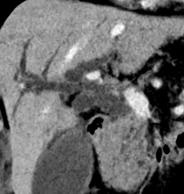
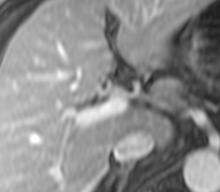
Multi-detector computerized tomography(MDCT)
TMD Teams
Intravenous contrast (multiple phases)
- MIP and MinIP reconstructions
- Oral biliary contrast or intravenous
- Rapid and accessible
Evaluates the BT proximal and distal to BO
Evaluates the BT and surrounding tissues
Excellent to determine
- Presence of BO (published data 81-94%)
- Level of BO (published data 88-92%)
Irradiation
Intravenous contrast (nephrotoxicity, allergy)
Not therapeutic
Tse, F. HBP (Oxford) 2006;8:409-25; Morosi C. Eur J Radiol 2009;72:114-7
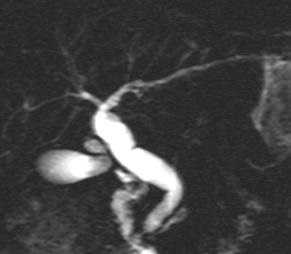
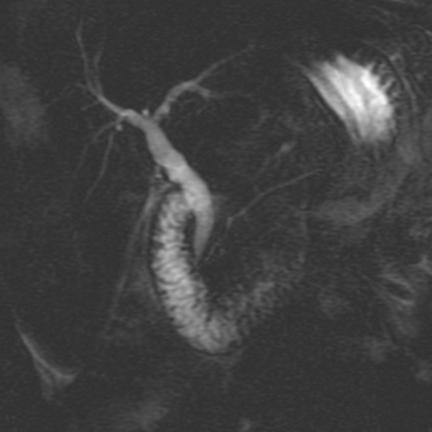
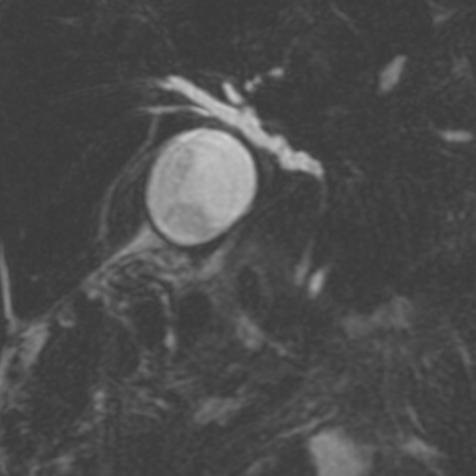
Magnetic resonance cholangiopancreatography(MRCP)
Cholangiogram s sequentials
- Rapidly acquired
Dynamic studies
- Extra-cellular contrast
Functional studies
- Biliary excretion of contrast (requires a certain grade of hepatic function)
Evaluates the BT proximal and distal to BO Evaluates the BT and surrounding tissues Excellent for determining level and cause of BO (Sensitivity 95%; Specificity 97%) Not therapeutic
Romagnuolo J. Ann Intern Med 2003;139:547-57.
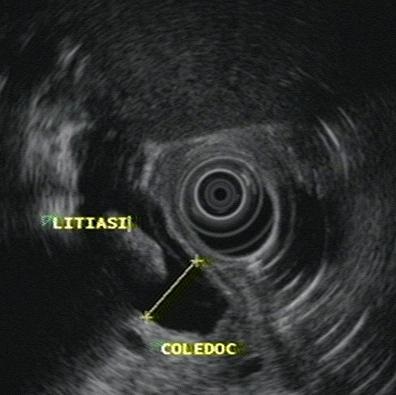
Endoscopic ultrasound (USE)Combines endoscopy and US
Diagnosis of the cause of BO
- Sensitivity 97%;
- Specificity 88%
Enables PAAF of neoplasias Operator dependent Not available in all centers Sedation
Interventional, or direct techniques
Endoscopic retrograde
|
 |
 |
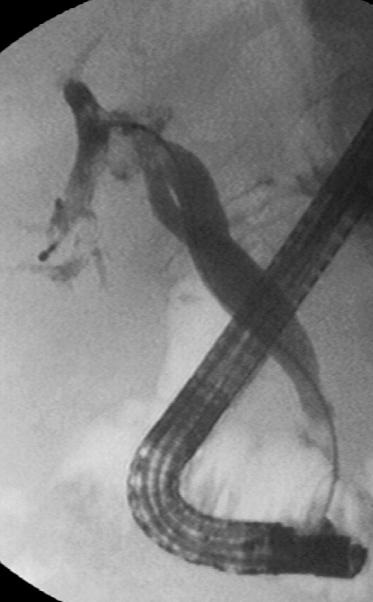 |
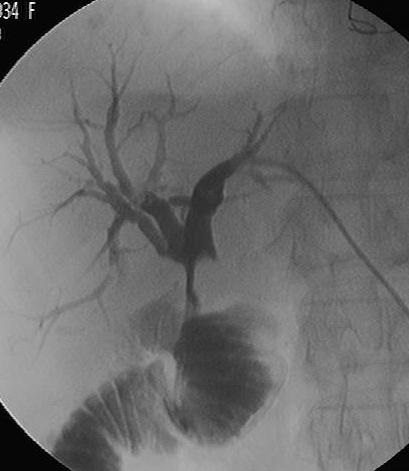
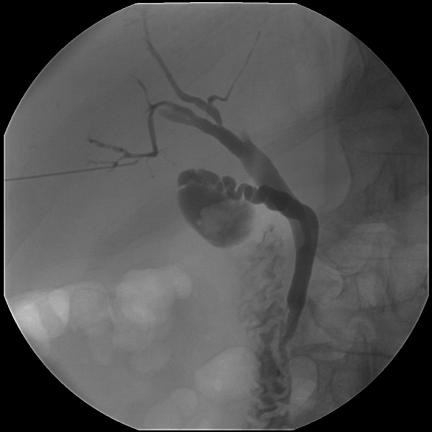
PTC. Advantages and indications
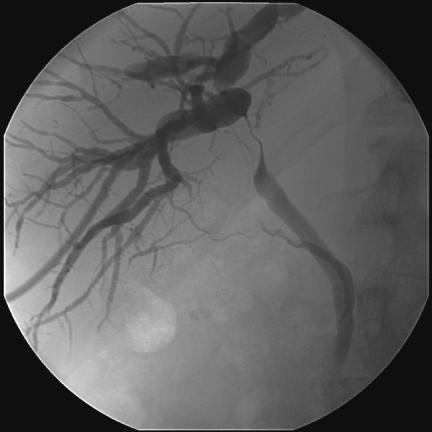
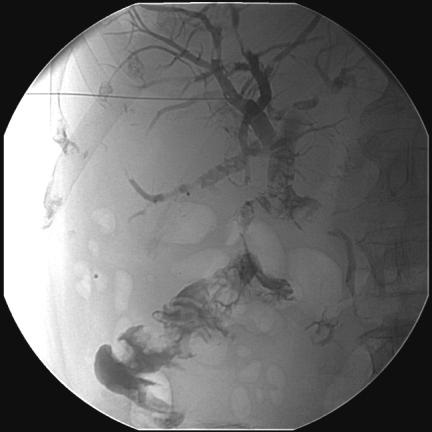
The biliary tree can be successfully visualized in close to 100% of patients with dilated ducts, and in 60-80% of patients with non-dilated ducts .
PTC is considered, along with ERCP, the gold standard by which all other imaging modalities of the biliary tree are evaluated. It is excellent at determining the level and cause of biliary obstruction, as well as distinguishing benign from malignant lesions, while being less costly than
ERCP.
It can also be applied therapeutically for external drainage of obstructed ducts and constitute a first step in the management of benign stenosis (balloon dilatation), metallic stenting for palliation of malignant lesions and percutaneous stone removal.
In all these scenarios, the overall complications and mortality rates are low in relation to the benefit obtained by the patient. Although nowadays
its use in scheduled procedures is indicated for patients whom ERCP has failed, incomplete or not available or when altered anatomy (gastroenterostomy) precludes accesing the ampulla , it also been increasely used in urgent situations (cholangitis or biliary sepsis , many times
after ERCP precisely), and especially to treat obstructive jaundice in hiliar tumors and to manage hepatolithiasis
 |
 |
 |
 |
 |
 |
PTC. Complications
The main concern with these techniques is the risk of complications inherent to these procedures; pancreatitis, cholangitis, perforation, bile leaks and bleeding that happens in about 8 to 12% of the cases and an associated mortality rate of 0.5-1% , for ERCP and about 2.5% of major complications for PTC following by biliary drainage, and a associated mortality rate of 1%.
Operative cholangiography (OC)
Tse, F. HBP (Oxford) 2006;8:409-25
JVIR 2003; 14:S243-S246
次
次